FHIR Standard: The Crucial Healthcare Data Solution for Secure Interoperability
- What Do Fast Healthcare Interoperability Resources Mean?
- So, Who Uses FHIR?
- But Is FHIR Interoperable with Other Healthcare Standards?
- Why FHIR standard is Important for Healthcare Providers
- Benefits of FHIR in Healthcare IT
- Considering Developing a Healthcare Solution?
- EHR Integration: How Technology Can Help Improve Healthcare Outcomes?
- How FHIR Works Across Healthcare Organizations
- What are FHIR Resources, and How Do They Function?
- Must-Know Fundamentals of FHIR Interoperability
- How Health Entertainment is Transforming Mental Healthcare
The healthcare industry has experienced several technological advancements in the last few decades, most of which have reduced costs and increased efficiency.
However, one area that continues to receive attention from tech giants is healthcare information interoperability.
The health data generated by various sources must be shared within a patient’s care plan and across multiple systems and database environments. But this can only be possible with some industry-standardized set of rules.
_1677166916.png)
Enter FHIR – short for Fast Healthcare Interoperability Resources.
This blog post will explore FHIR in detail and explain why healthcare organizations increasingly adopt FHIR standards.
HL7 INTEGRATION: A REFERENCE FOR ITS BENEFITS, IMPLEMENTATIONS, AND APPLICATIONS
What Do Fast Healthcare Interoperability Resources Mean?
Fast Healthcare Interoperability Resources (FHIR) refer to healthcare data standard developed by the HL7 organization that enables secure, real-time health data exchange across disparate healthcare organizations.
The ultimate goal of FHIR is “interoperability,” meaning all digital products within the healthcare ecosystem can exchange information with one another regardless of the vendor or system used.
FHIR is used by healthcare providers, payers, technology vendors, and other stakeholders in the healthcare industry. It is especially popular among developers of healthcare applications, as it offers a flexible and easy-to-use standard for exchanging data.

Yes, FHIR is designed to be interoperable with other healthcare standards, such as HL7 v2 and CDA. It is also being used in conjunction with emerging technologies like blockchain and artificial intelligence to improve healthcare interoperability and data exchange.
Why FHIR standard is Important for Healthcare Providers
FHIR is an important standard for healthcare organizations because it enables the secure exchange of electronically-protected health information across systems and providers. Different data formats can be exchanged through FHIR.
This standard can help remove data silos created over time by disparate IT systems across multiple departments within a hospital system.
Let’s look at the key benefits of FHIR in the next section.
FHIR provides a standardized way for health systems, patients, physical records providers, and other healthcare applications to interact securely. It makes data sharing across different platforms in real-time more manageable. This can reduce the time required to access particular medical histories or test results within one system from multiple sources.
WHAT IS EHR (ELECTRONIC HEALTH RECORD), AND HOW DOES IT WORK?

FHIR enables faster clinical decision support through near-instantaneous exchanges of the requested information, such as clinical data that may be required before a physician makes diagnosis/treatment decisions.
FHIR enables healthcare professionals to rapidly access patient information from multiple electronic health records (EHR) software systems by connecting different platforms. This helps reduce time lags arising from cross-platform implementations, allowing healthcare professionals to access vital client details remotely conveniently and timely.
THE HEALTHCARE ECOSYSTEMS: A TOUR THROUGH THE HEALTH-INTERCONNECTED WORLD
Data standards defined by FHIR are instrumental in enhancing security protocols and ensuring compliance with HIPAA regulations. The open APIs offered via cloud technologies enable administrators to manage access to data, thereby aiding in the protection of sensitive patient information and safeguarding patient privacy.
FHIR’s well-defined terminology ensures everyone on a health IT system can understand what different components mean. This significantly speeds up how quickly clinical care is delivered, improves accuracy, and minimizes misunderstandings due to the ambiguity of non-cross-deployed API architecture implementations.
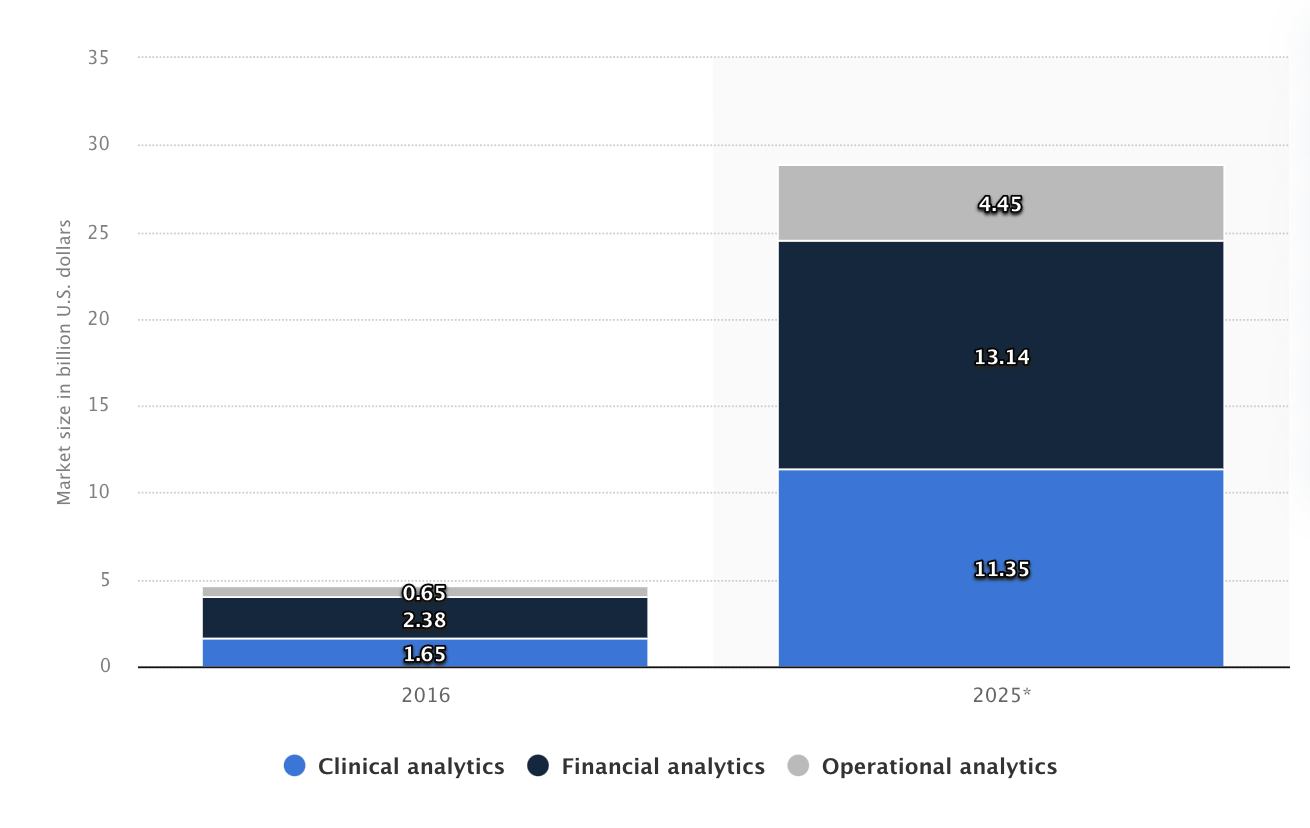
According to Statista, by 2025, the market for health-related financial analytics services using big data will increase to over 13 billion U.S. dollars. For organizations to be market-ready in the future, they must implement an efficient analytics system. FHIR also helps them because it allows for accurate longitudinal tracking of medical records within standards.
This means healthcare organizations can leverage algorithmic-based machine intelligence tools to track disease patterns or other variables like appointment attribution automatically.
Improved data analytics also enable better planning/forecast decisions regarding resource allocation over time, resulting in financial savings and efficient use of personnel services.
If you want to know more about HL7 FHIR integration, you should definitely listen to our CareMinds podcast, particularly the episode with Redox specialist Nick McKenzie.
Nick went on to work with the EHR integration architecture, which he compares to building a house, where an entire team of contractors, roofers, electricians, and plumbers work cohesively under an architect.
“I was always fascinated with this idea of being the translator helping clinicians translate their requirements into what they wanted the system to be designed and then translating back to the technical teams how to execute and interestingly enough. It’s all that product management really is.”
Watch other episodes as well!
PODCAST #3. HOW TECHNOLOGY CAN HELP IMPROVE HEALTHCARE OUTCOMES
How FHIR Works Across Healthcare Organizations
FHIR harnesses a modern, web-based approach to connect different healthcare systems, allowing data to flow effortlessly between them.
With its modular architecture, FHIR can adapt to the diverse needs of various healthcare organizations, from bustling hospitals to research institutions.
FHIR is built upon a set of resources, like building blocks representing standardized clinical and administrative data.
These resources are organized into modules, each representing a specific aspect of healthcare data.
TELEMEDICINE VS. TELEHEALTH: A COMPREHENSIVE GUIDE ON THE DIFFERENCES & BENEFITS
For example, the Patient module has patient demographics, medical history, and care team data. The Observation module captures information on a patient’s vital signs, lab results, and other information in clinical documents.
For healthcare organizations to exchange critical information in a secure manner using FHIR, they rely on an interoperability layer that transforms the data into a universal format. This layer is an FHIR server, which can be hosted locally or in the cloud. Healthcare organizations can easily access FHIR servers using standard internet protocols like RESTful web services and OAuth 2.0 authentication.
When one healthcare organization needs to exchange data with another, it sends a request to the other organization’s FHIR server. The proposal indicates the data types, and the server responds by sending the requested data in a standardized format.
The receiving organization can then use the data in its systems, such as electronic health records, decision support systems, or population health management tools.
TOP 10 HEALTHCARE TRENDS EXPECTED TO BE IN 2023
 1_1677167295.png)
What are FHIR Resources, and How Do They Function?
FHIR resources are structured documents and messages representing various health and medical entities.
The FHIR standard defines the structure and content of these documents, which include patient data, insurance claims and billing information, diagnostic and laboratory records, medication use information, and care plans.
These resources drive effective health information exchange between stakeholders, such as healthcare providers, insurers, and patients.
STEP-BY-STEP GUIDE ON MOBILE APP HIPAA COMPLIANCE
Must-Know Fundamentals of FHIR Interoperability
Here are four important things to know about FHIR interoperability basics:
- FHIR is built for modern healthcare: It was designed using the latest web technologies and follows a modular approach, making it more flexible and scalable than other healthcare data exchange standards.
- Flexible and customizable: FHIR resources can be easily extended to accommodate custom data elements and new use cases. This helps developers easily choose the components they require for particular use cases.
- Promotes data interoperability: It drives the free flow of healthcare data among different systems. This enables healthcare providers to coordinate care more effectively and allows patients to access their health data easily.
- Being widely adopted: Many major EHR vendors and healthcare organizations already use FHIR-based solutions because of their ease of use and ability to support modern healthcare workflows.
_1677167348.png)
How Health Entertainment is Transforming Mental Healthcare
Health entertainment transforms mental healthcare by providing activities and games to improve relaxation, exercise the mind, or provide other forms of therapy.
These health-themed interactive programs are meant to divert from everyday stressors while helping people recognize signs of depression and seek help more enjoyably. Health entertainments often focus on creating positive experiences with wellness information through:
- Music listening parties that promote self-care strategies.
- Guided audio stories that explore mindfulness skills.
- Videos that highlight new perspectives on relationships between emotion regulation techniques, understanding trauma, and resilience-building resources coupled with quality physical activity instruction.
The physical activity instruction is specifically designed to address concerns about body image.
KEEP A PULSE ON EPIC APP ORCHARD AND HOW IT BENEFITS THE HEALTH SYSTEMS
Conclusion
The FHIR standard is a positive approach to data communication and interoperability for the healthcare sector. It provides an efficient way to access, share, and manage health data in various settings.
Now that you have learned about its features and benefits, it’s time to ensure that your organization takes advantage of this technology as quickly as possible.
Organizations can improve healthcare outcomes by leveraging the FHIR Standard through effective security protocols such as authentication methods or encryption technologies while ensuring medical information’s safe transmission and accuracy.
