Healthcare apps development: types, examples, and features
- mHealth market overview and trends
- Steps of healthcare app development services
- Types of mobile health apps
- Professional healthcare app
- Want To Build a Healthcare Mobile App?
- Healthcare mobile apps for patients
- Build Your Own Dedicated Team
- Regulations to consider before starting a healthcare app development
- Ready to hire a healthcare app development team?
- Success Story of The APP Solutions
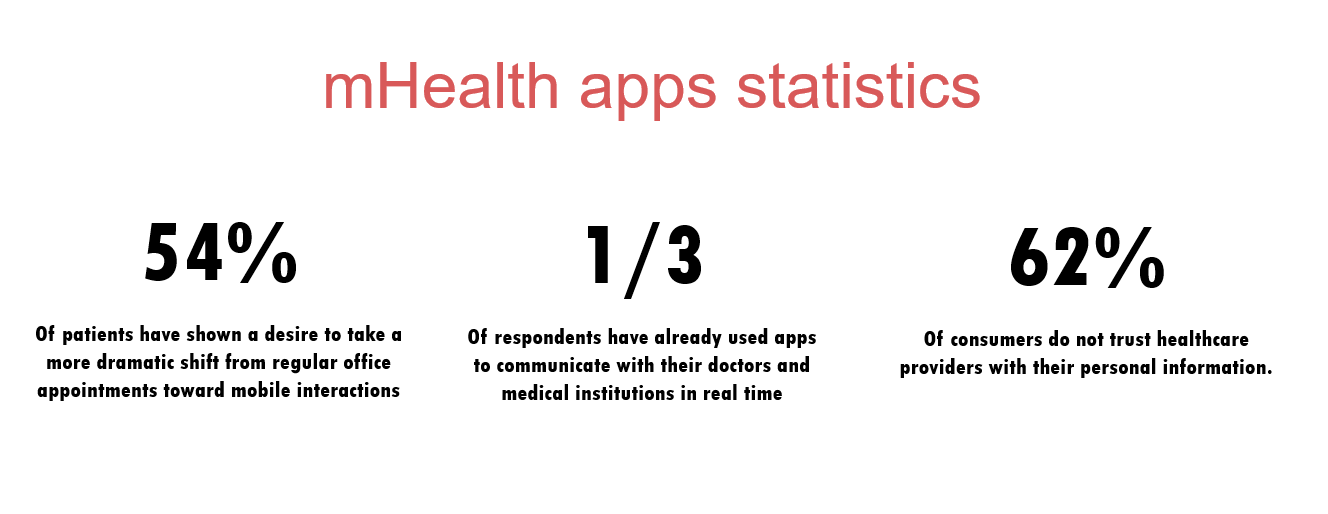
The industry of mHealth is up and running and there are now over 350,000 digital healthcare apps available to consumers in the App Stores. There are numerous mobile medical apps for different purposes, including health data analytics, appointment booking, telemedicine, and even meditation – yes, the healthcare industry is expanding by leaps and bounds.
With such diversity, you can use your device, not only for tracking the number of calories burned, but also to receive consultation from a medical specialist or predict various medical conditions.
If you are looking for a healthcare app idea for further healthcare apps development, you are in the right place. Below we list the most prominent healthcare apps for doctors and patients with examples and explain how to make the mHealth app compatible with essential regulations across the globe.
But first, let’s take a quick look at the healthcare apps market and healthcare providers.

How To Make A Medical App In 2022: The Ultimate Guide
mHealth market overview and trends
Healthcare mobile apps revolutionize the way patients receive medical treatment and monitor their medical conditions. Building a health app develops accordingly.
- Statistics show that there are currently over 325, 000 health-related mobile health apps now presented on app marketplaces.
- Statista reports, in 2020, the healthcare app market is expected to reach 60 billion U.S. dollars.
- 60% of mobile device users downloaded a mHealth app to their device.
- As for healthcare mobile app trends, mobile fitness apps are more popular among Android users (39% of download), while iOS users prefer using health-oriented medical apps (62% of downloads), that are convenient to use via Apple Watch.
- At the same time, mobile healthcare apps increased productivity among medical staff and clinicians, and are expected to save over $200 billion on remote patient monitoring.
Now that you are aware of the main mHealth app market trends and stats, let’s find out more about the healthcare app development process so you will know how to build a healthcare app.
Related readings:
Calmerry Online Therapy Platform
Orb Health – Сare Management As A Virtual Service
BuenoPR – 360° Approach to Health
Steps of healthcare app development services
Step 1. Choose your technological partner among healthcare software development companies
When choosing the best healthcare dev company, consider previous projects, client reviews, and the company’s tech expertise. Develop a healthcare app is a process that will take more than a month, so it is very important that both the contractor and the customer feel comfortable.
Step 2. Ask developers for a quote to create a healthcare app
Fill in the contact form to schedule a meeting with a business development manager to clarify more details of your project.
Step 3. Receive a rough estimate on medical app development
Based on the project’s details, a business analyst, project manager, and solutions architect will create a rough estimation for your project and send it to you.
Step 4. Launch the inception phase with a team of healthcare app developers
When you agree on the initial estimation, healthcare app developers will clarify more details on your project to create user stories, mockups, and wireframes.
Step 5. Start the healthcare software development process
When you agree on all deliverables of the inception phase, the team (tech stack) will start healthcare mobile application development iteration by iteration.
WHY CREATE A CUSTOM MENTAL HEALTH APP IN 2022
Types of mobile health apps
There are different types of medical apps aimed at various end-users, including healthcare professionals, labs, and patients, which impact their features, some integrations, and the degree of data security required. Let’s talk about the most popular healthcare apps.
Professional healthcare app
Targeted at medical personnel, such apps include patient data, such as name, date of birth, insurance number, address, and so on. Thus, when launching a professional healthcare development process, you need to make a healthcare app HIPAA compliant and pay extra attention to private data encryption to avoid data breaches. mHealth apps for medical specialists include the following types:
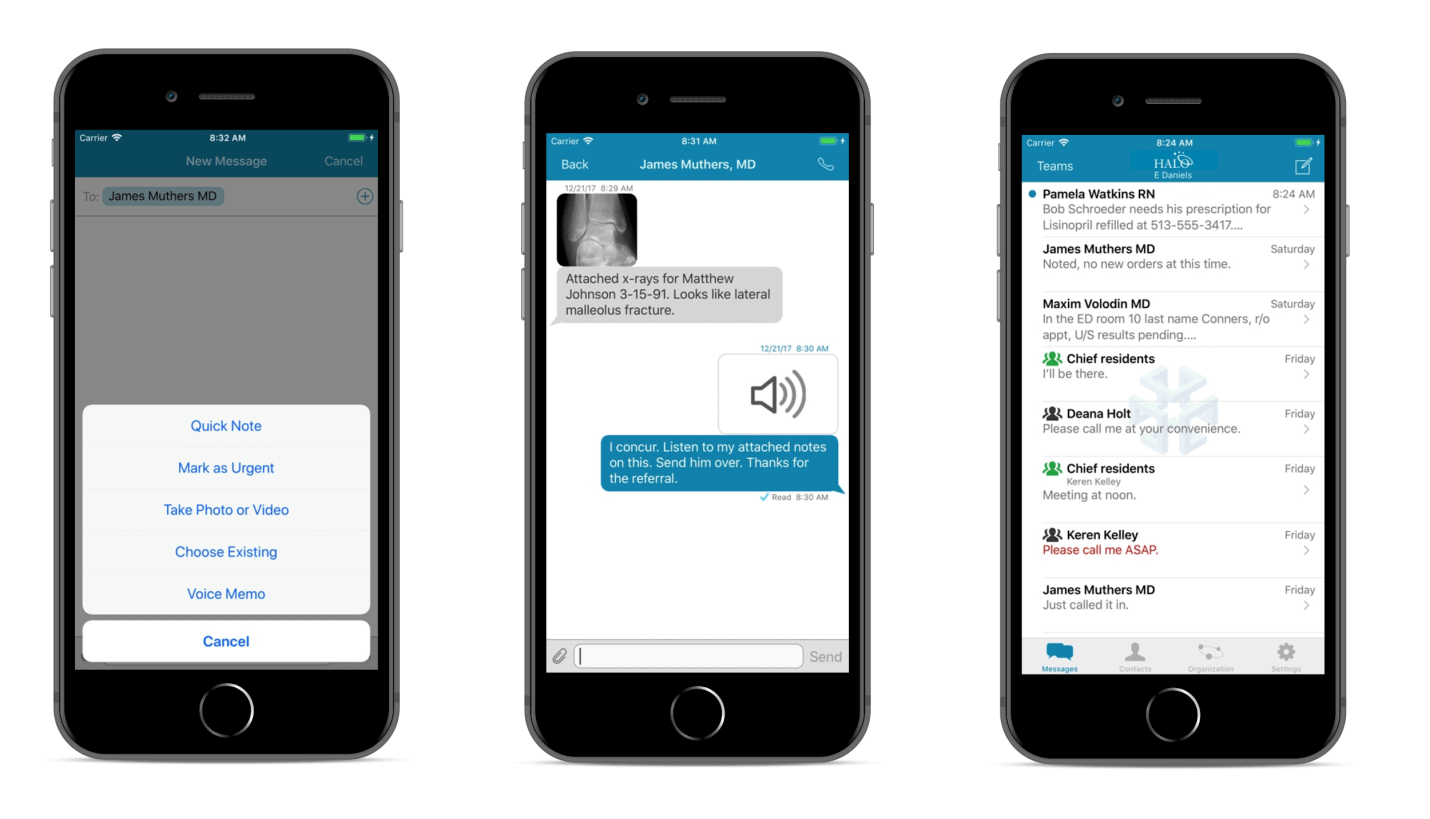
Clinical communication apps
Such health apps are developed to improve clinical decision-making and communication with clinical specialists in a particular hospital. They include messaging and voice chat, file sharing, and electronic health record systems.
One example of such a healthcare app is Halo, a communication, and collaboration platform for clinical specialists, which includes the following features:
- Send physicians and nurses Lab and PACS results
- Integrate with EHR (electronic health records) to edit patient records in real-time
- Store files on a cloud-based platform, Amazon Web Services
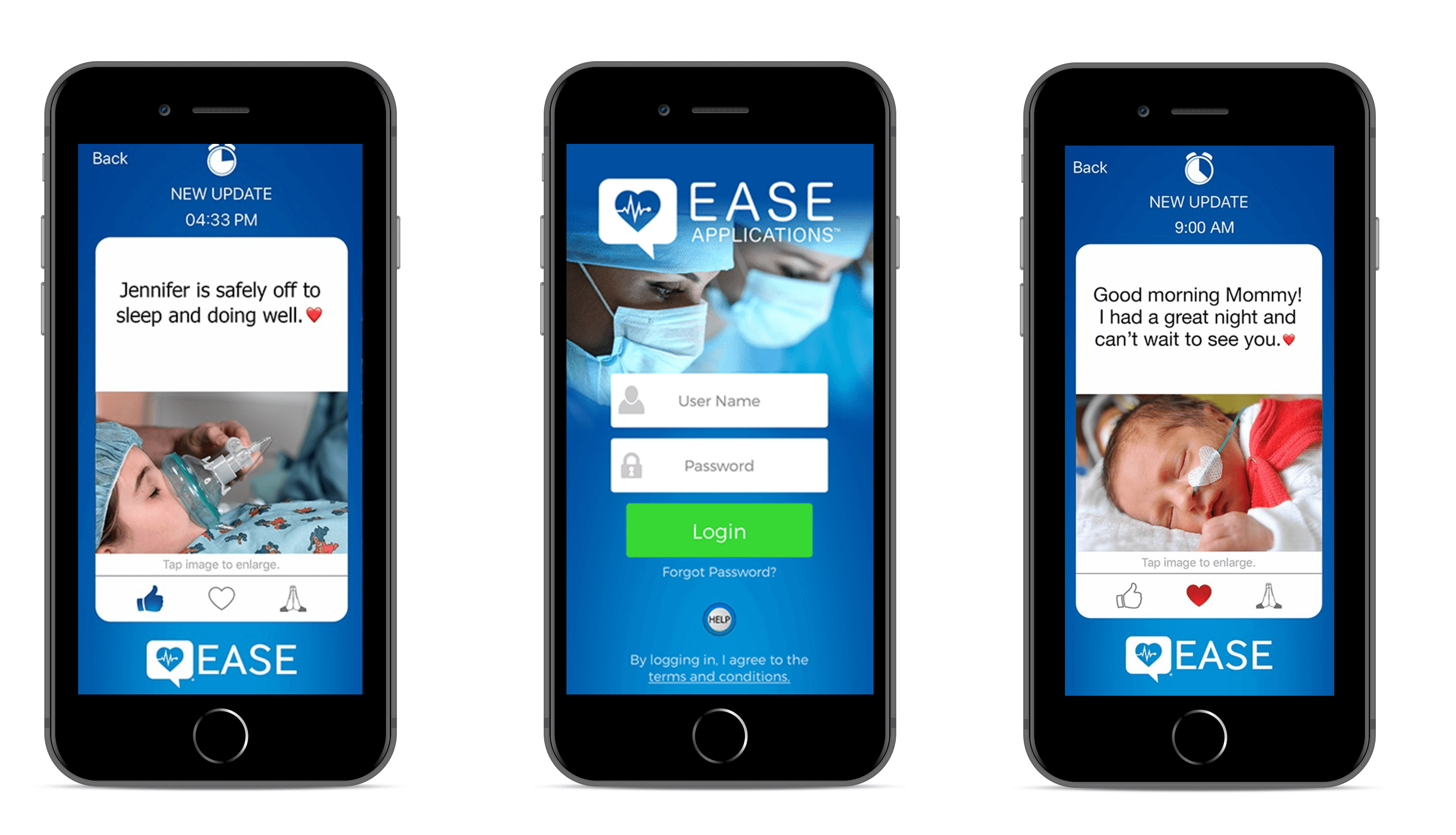
Patient communication apps
This type of healthcare app boosts customer satisfaction, loyalty, health outcomes, and provides more transparency between patients and doctors.
That is how the EASE mobile app works, offering users the following features:
-
- Invite relatives to the network within the healthcare app to keep them informed about updates
- Include HIPAA compliant texts, photos, and videos that will self-destruct after 60 seconds
- Send premade bulk messages to patients and their families to keep them informed
- Prohibit saving files, texts, or other documents from the healthcare app to the device to ensure patient privacy and avoid data breaches
Need help in developing your Healthcare App?
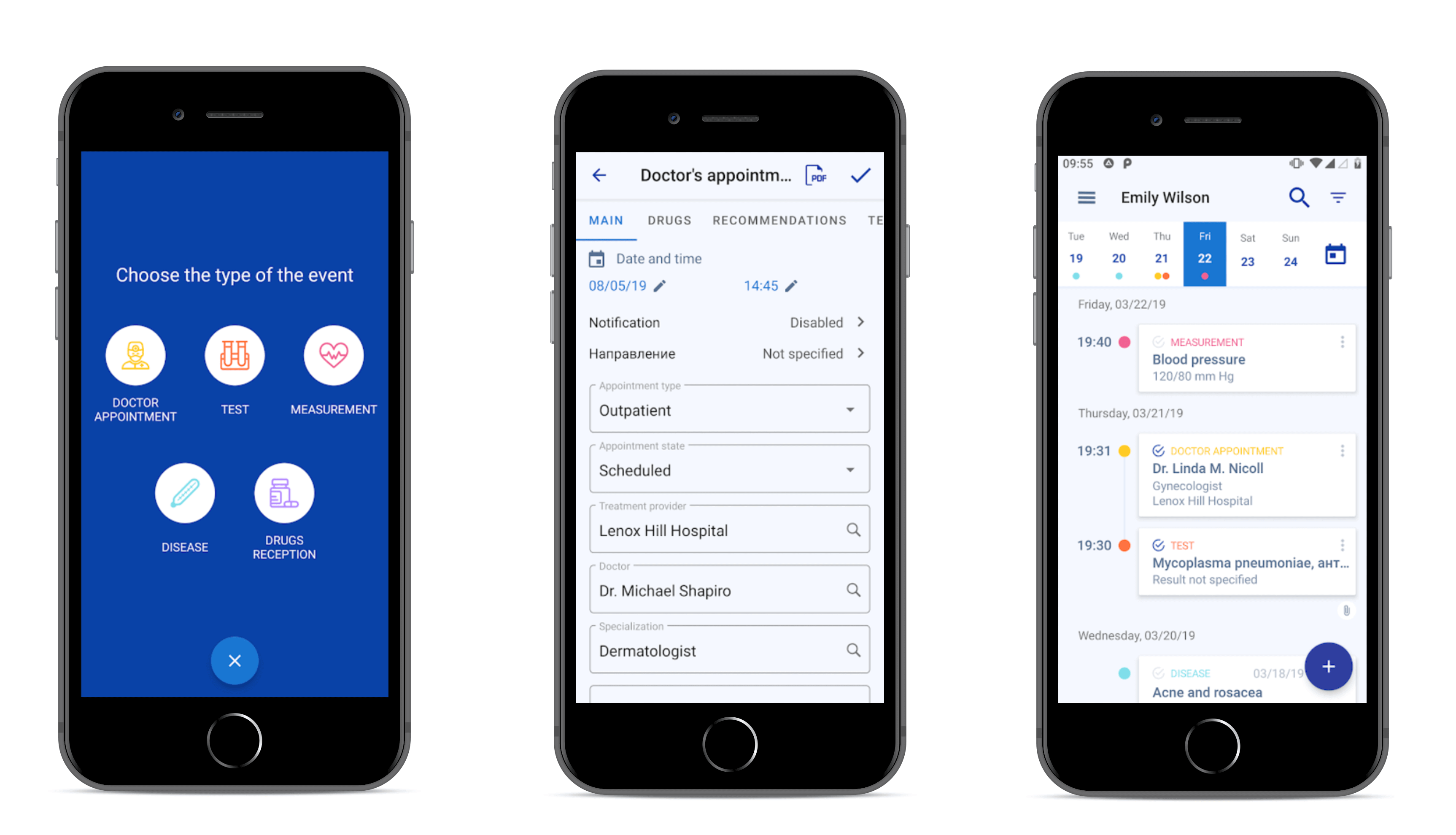
Reach outMedical record apps
Such health apps simplify updating patient records, including blood pressure, medical visits, examinations, prescriptions, and other information to keep track of a patient’s progress.
Medical Record is a healthcare app that belongs to this category. In addition to the features above, the app also includes:
- Prescription module allowing doctors to save medical info
- Appointment feature to schedule an appointment with patients
- Recording videos or procedures instead of text messages
- Searching patients by I.D.
Risk assessment apps
Such health apps are integrated with Electronic Health Records (EHR) and wearable devices, which allows monitoring patients’ health conditions in real-time, tracking heart rate, and identifying patients at risk. To build a risk assessment mobile app, developers often use machine learning for pattern recognition, as we did for our recent project, a skin cancer detection neural network.
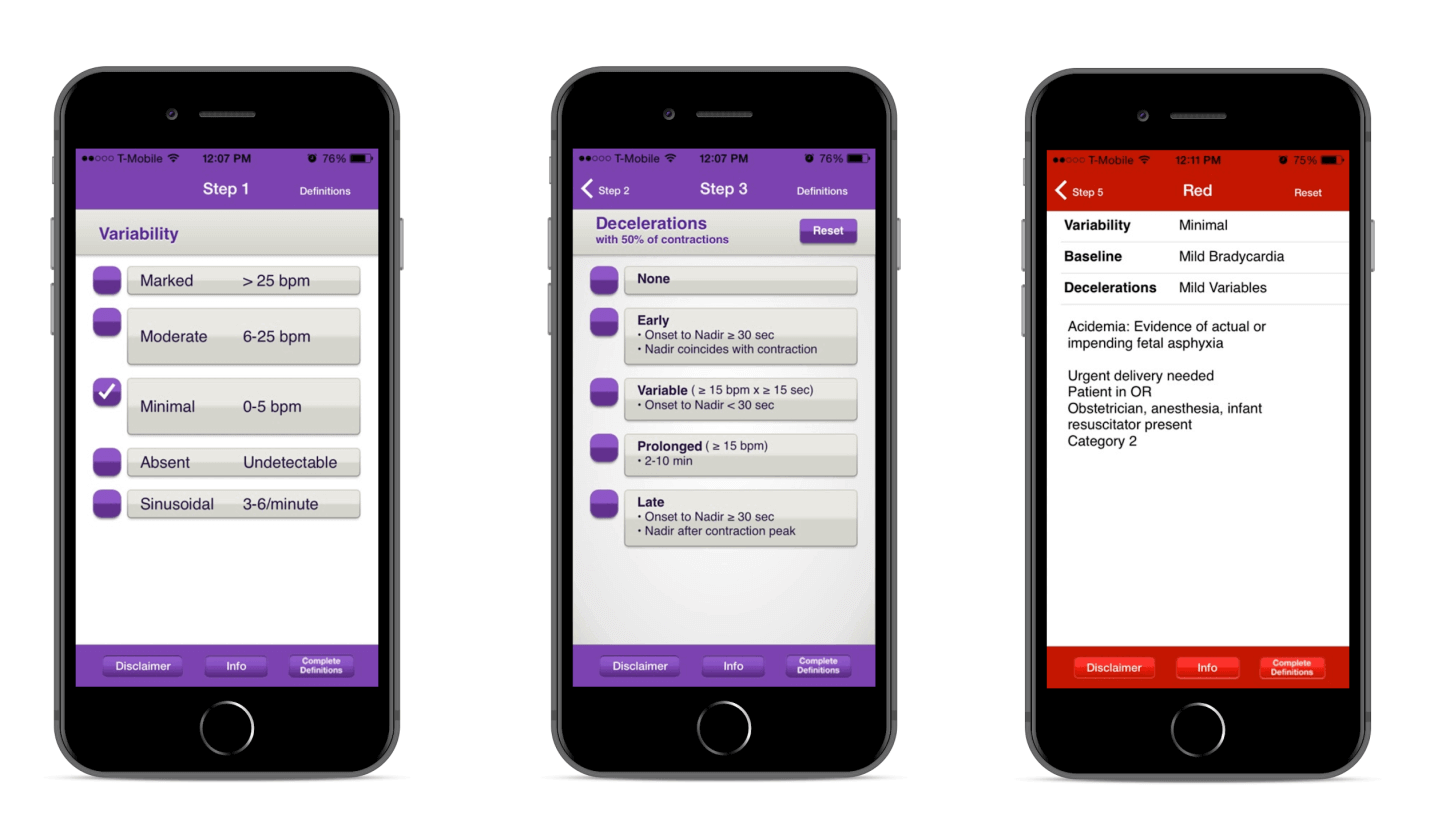
An example of such a medical app is FHR 5-Tier(Forecast Health Risk and Predication), aimed at obstetricians, midwives, and nurses who use electronic fetal monitoring (EFM) for patients in labor. Let’s look at its features:
- The healthcare app allows interpreting fetal heart rate (FHR) tracings to decide about further patient treatment in real-time
- The five-color (green, blue, yellow, orange, and red) system is used in the medical app to allow medical specialists to standardize the management of different fetal heart rate tracings.
- When the healthcare app finds a risk to a patient’s health, it uses colors Yellow, Orange, or Red to notify the doctor about the patient’s state of urgency and provide a list with recommended actions.
Barcode Scanning apps
Barcode scanning apps in healthcare allow scanning a patient’s electronic health records and medication barcodes using a built-in camera in their mobile devices, avoiding expensive barcode scanning devices.
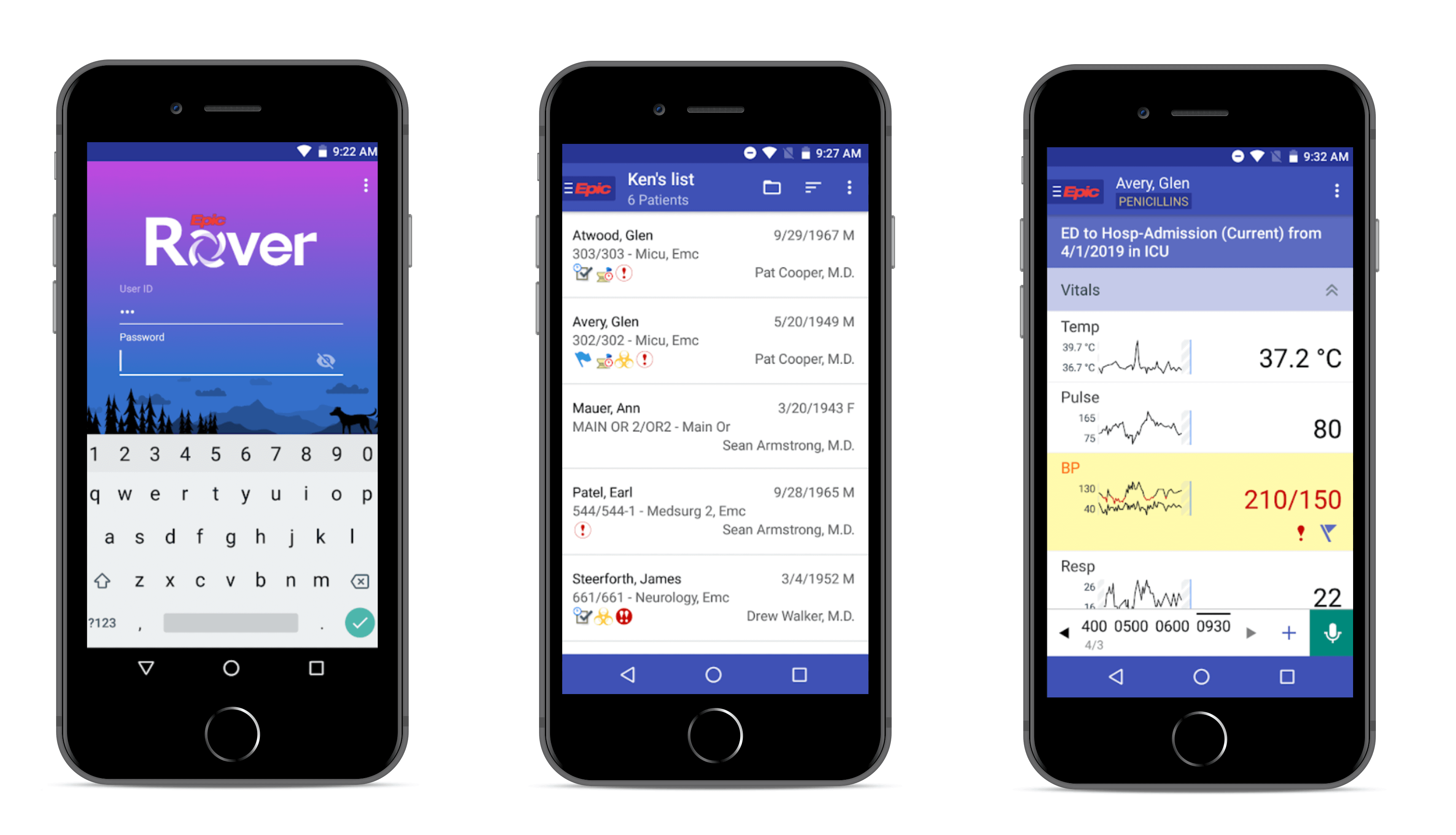
Epic Rover is one healthcare app that belongs to this category, empowered by Scandid Barcode scanner SDK. Apart from scanning a patient’s medications barcodes, develop a healthcare mobile app with the following features:
- Integration with Epic electronic health records for better admission of medicines and treatment
- Visualization of patient-related info and progress in the form of charts
- Build-in messenger to communicate with patients and other medical personnel
And other functions to make the doctors’ work even more efficient.
KEY DIFFERENCES IN EHR VS. EMR VS. PHR: WHAT TO CHOOSE FOR YOUR HEALTHCARE ORGANIZATION
Medication dosage apps
Such applications are used by physicians to calculate individualized doses of medicine based on the patient’s age, weight, and other personal info, avoiding laborious manual calculations, spreadsheets, and sophisticated tools.
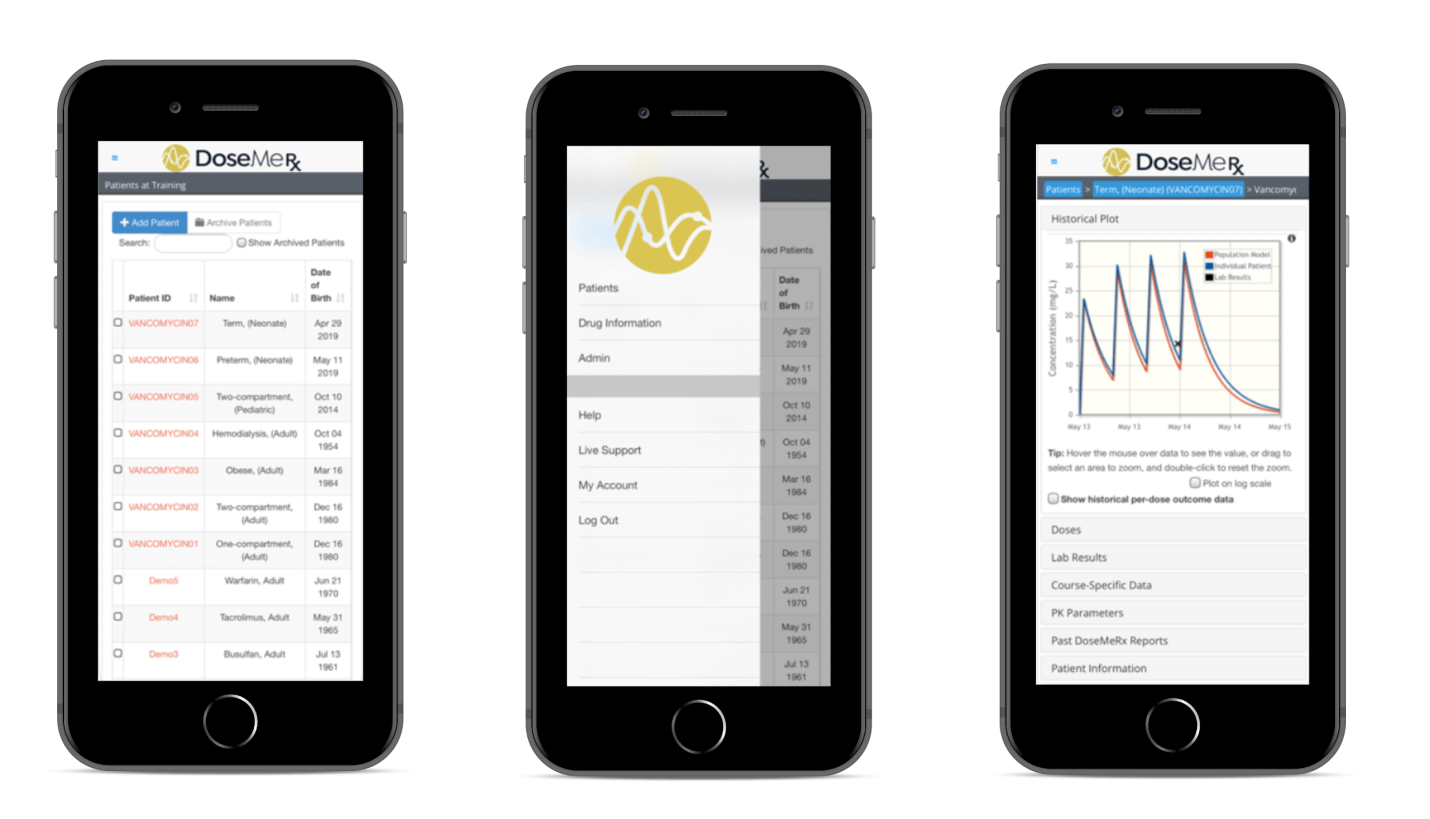
One example is the DoseMeRx app for such a target audience as healthcare professionals. Let’s find out more about this mobile healthcare app:
- Integration with EHR, where the doctor can leave notes on the patient’s state, medications, and dosage assigned
- Set up reminders so that patients can track their medication intake
- Build-in feature to predict treatment outcomes
- Integrated dose optimization feature that leverages Bayesian dosing methods to guide dose optimization, based on clinically validated pharmacokinetic drug models, patient characteristics, drug concentrations, and genotype
READ ALSO:
Hospital Mobile App Development
Healthcare mobile apps for patients
The patient-oriented mobile healthcare industry includes two main categories: medical and wellness. Below, we highlight every type of medical app from both of these groups, their examples, and essential features.
Doctor-on-demand or Telemedicine apps
Even in a busy environment, patients can receive treatment and consultations from medical specialists using telemedicine apps, without leaving their offices or homes. Such mobile health application helps patients to find a necessary medical specialist from a pool of doctors, book an appointment, and attend it via video call and pay for the consultation via an integrated payment gateway.
A GUIDE ON HOW TO CREATE A TELEMEDICINE APP LIKE DOCTOR-ON-DEMAND
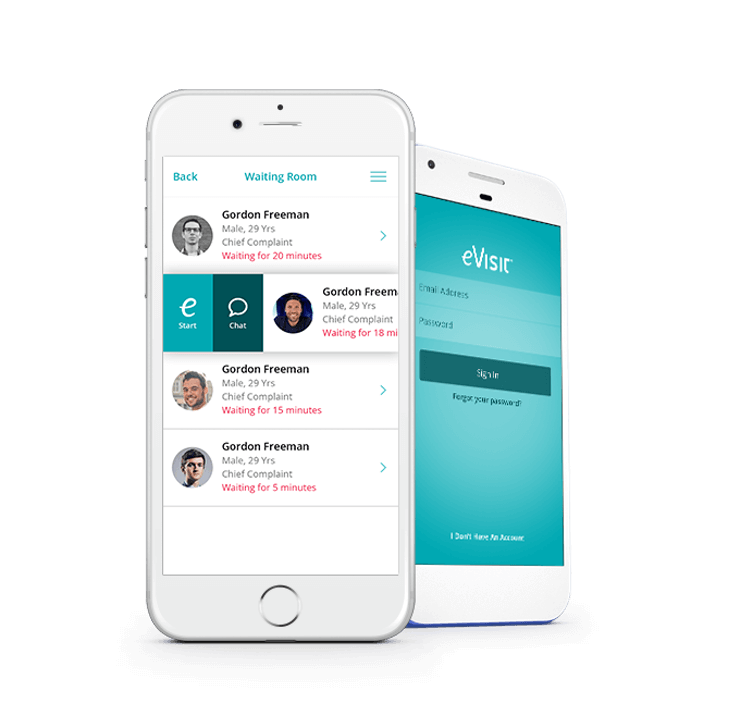
One typical doctor-on-demand mobile app is EVisit that includes other features:
- Virtual waiting room with waiting time tracking where patients can prepare the information required
- Two-way video connection so patients can see the doctors they communicate with
- Built-in messaging, EHR, search for medication, prescriptions, and other features to deliver patients the medical experience of attending an offline appointment with a doctor.
[Source: Softwareadvice]
HOW THE HEALTHCARE INDUSTRY BENEFITS FROM HYBRID CLOUD SOLUTIONS
Condition-based apps
Such apps are popular among users with epilepsy, diabetes, cardiovascular disease, asthma, allergies, and even depression. While some apps in this category are more sophisticated versions of a digital diary with visual medication management, others use predictive analytics and machine learning to notify a user about a particular health condition one should be aware of.
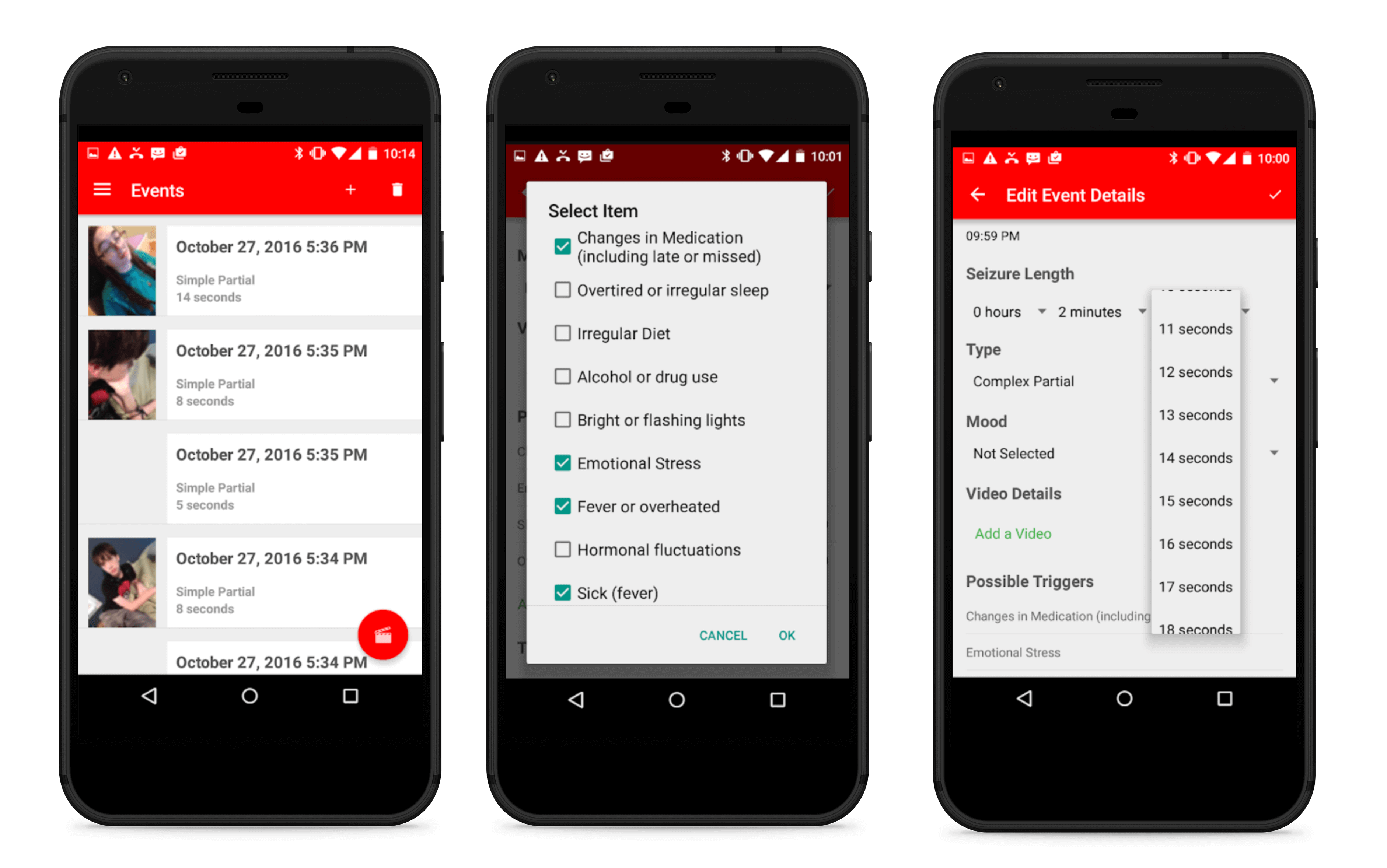
Founded by Munroe-Meyer Institute, Seizure Tracker is a perfect example of apps that allow users to log their seizures, and includes a bunch of other features:
- Video recording, so patients can describe their seizures, their triggers, and what happened afterward
- Manual input of seizure info, so the user can specify their seizure type, time of day, length of the seizure, and other related information
- Option to synchronize user profile with private Youtube channel to record info about seizures and share it with relatives
Fitness apps
Such a health app help users keep fit by tracking their daily activity, weight, number of calories burned, a list with workout programs, and integration with wearable devices. In our previous article devoted to fitness app development, we described other features of such apps and gave you a guide on how to develop one.
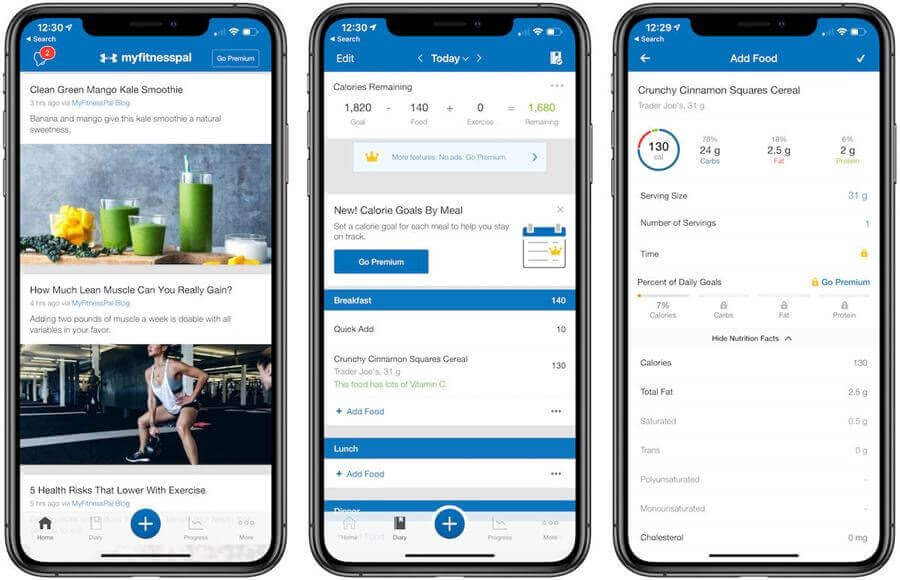
MyFitnessPal is the most popular fitness mobile app, which includes:
- Diet tracking with recommendations on calorie consumption based on the user’s age, weight, sex
- User community where other users share their success stories about losing weight
- Calorie counter to control the amount of food, water and coffee consumed
[Source: Fusioninformatics]
I want a free consultation for my Healthcare project
Contact UsDiet and nutrition apps
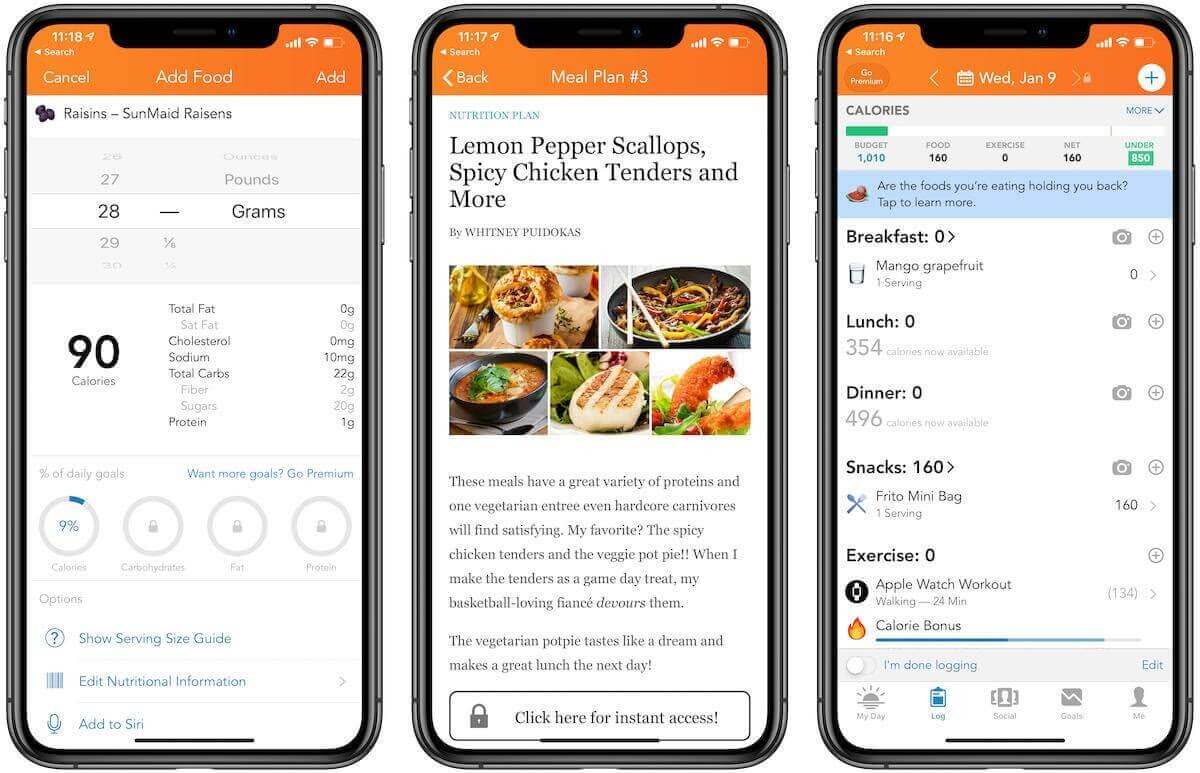
Diet and nutrition apps are another popular category in the mHealth market, targeted at users who want to lose weight. The standard set of a diet app includes a comprehensive library with food and nutrition, a calorie counter, a diary with meals, and a progress chart.
Lose It! app belongs to this mobile app category and provides users with the following features:
- Barcode scanner to receive information about product nutrients within seconds, and track intake of carb, macro, and calorie
- Snap It allows users to log images of food taken on a mobile device
- Meal planning to customize the user’s eating and track macro, carb, protein, and overall calorie intake
[Source: Macworld]
HEALTHCARE CYBERSECURITY: HOW TO PROTECT PATIENT DATA
Meditation apps
Meditation mobile apps also belong to the mHealth market since mental health apps help users to maintain their psychological states with the help of guided meditations. As a rule, such healthcare apps include a library with pre-recorded sessions of guided meditations, timer, gamification, and useful tips about breathing exercises.
Calm, the best-known meditation mobile app, valued at $1 billion, helps users reduce stress and improve sleep. To achieve these goals, they use not only ancient methods of relaxation, but also a scientific approach based on ongoing studies conducted by scientists from Arizona State University, Ryerson University in Toronto, Massachusetts General Hospital, and others.
The main features of the Calm app are:
- Guided meditations for different purposes (relationships, breaking habits, happiness, etc. )
- Mediations of different lengths for users with varying levels
- A library with podcasts, sleeping stories, relaxing music, breathing programs, and masterclasses

STEP-BY-STEP GUIDE ON MOBILE APP HIPAA COMPLIANCE
Regulations to consider before starting a healthcare app development
If you want to build a mobile medication app, things to consider are security regulations and compliances across different countries that are mainly concerned with patient data safety. Otherwise, if your app does not meet these regulations, no matter how good your health app is, it will be deleted from app marketplaces.
The good thing is to build a weight loss, calorie counter, or meditation app, you do not need to make it compliant. For other mobile applications that deal with a patient’s health records, and other sensitive personal data, you need to consider the following regulations in order to keep user’s medical services data safe from breaches:
The USA
The law requires health app developers to ensure, not only application security from any third parties, but also sensitive patient data stored on the mobile device or during big data transmission.
This regulation requires any health status information, including the provision of health care, or payment for health care, health plans, and other information that can be linked to a specific individual, to be secured and protected from third parties.
This act contains expanded privacy and security provisions that were included under HIPAA, also holding their business associates and service healthcare providers responsible for disclosing breaches. The bill is aimed at addressing the privacy and security concerns associated with the electronic transmission of health information.
THE APP SOLUTIONS – CUSTOM HEALTHCARE SOFTWARE DEVELOPMENT COMPANY
The European Union
To launch your mHealth app on the European market, you should provide users with the ability to protect and control their private information concerning the processing of personal data.
This directive protects the rights and freedoms of persons concerning the processing of personal data and the movement of free data.
The United Kingdom
The Data Protection Act (DPA) is a United Kingdom Act of Parliament, which controls how organizations, businesses, or the government, use personal information. It protects people and lays down rules about how data about people can be used.
Canada
The act governs how private-sector organizations collect, use, and disclose personal information in the course of commercial business. At the same time, it states that people should have access to their data held by any organization or business, with the right to challenge its accuracy. Appropriate safeguards must protect personal information.
HOW TO MAKE EHR/EMR EPIC INTEGRATION WITH YOUR HEALTH APP
Ready to hire a healthcare app development team?
There are many types of mHealth apps aimed at different users. If you are going to develop a healthcare app, you need to consider its end-user, since it impacts the number of features, as well as regulations to consider. If you are looking for a healthcare mobile app development company, want to receive further consultation, or estimate the app’s cost, drop us a line.
Success Story of The APP Solutions
Calmerry Telemedicine Platform Case Study
Our main goal for the Calmerry project was to develop a secured platform that brings together patients and licensed clinical psychologists via online counseling and chat room. We wanted the online therapy platform to be equally useful for both patients and therapists giving them a secure therapy space.
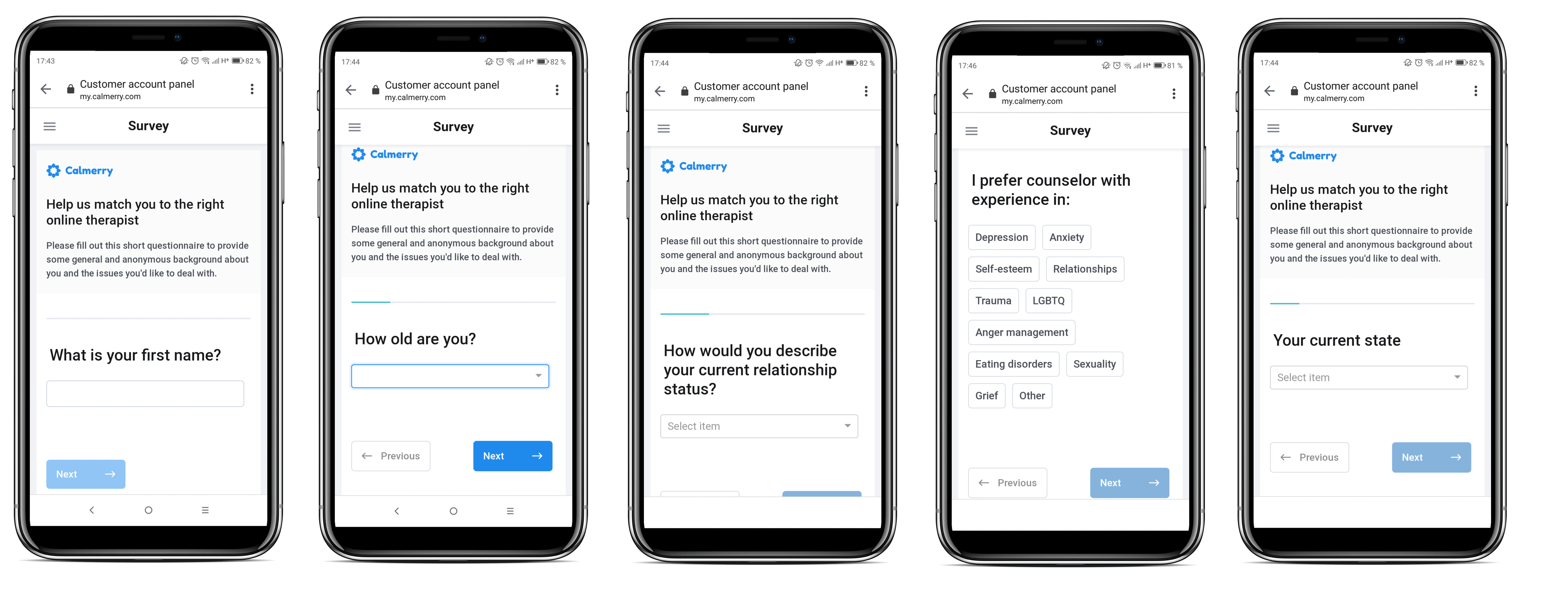
We delivered a GDPR-compliant e-therapy platform with essential functionality. You can see the project’s website on the link.
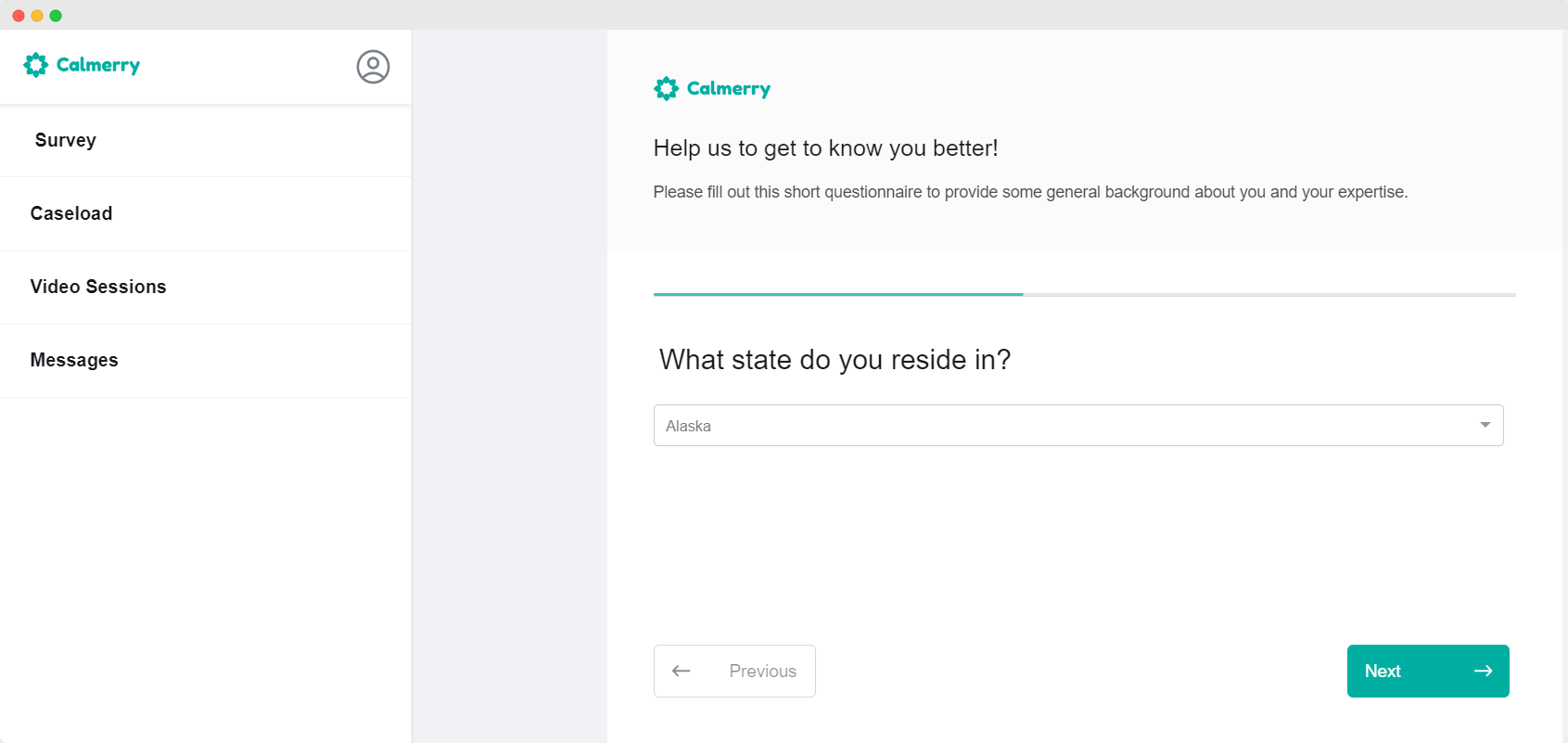
After delivering the first version of the Calmerry online therapy platform, we started to create the next project version. Right now, we are improving the user experience for patients and therapists, integrating therapist notes into video chat, and session booking via a calendar. We are also considering enabling file exchange via a messenger between users.
Download our Free Healthcare app eBook
Download
